Diagnosis & Prevention of Pressure Sores
Pressure sores are preventable injuries that often affect those with limited mobility. Early detection and understanding of risk factors are key to effective care and better outcomes. Explore causes, stages, and expert tips to protect yourself or your loved ones.
An Attorney’s Insights and Advocacy Journey
Join attorney, Kelley Simoneaux, as she shares her personal story of living with a spinal cord injury and her dedication to helping others. In this video, she explains the stages of pressure injuries, offering insights, awareness, and hope for those navigating similar challenges.
Step-by-Step Guide to Early Detection and Prevention
Perform Regular Skin Checks
Inspect the skin daily, paying particular attention to bony areas such as the sacrum, heels, and elbows for any signs of redness, changes in texture, or other abnormalities that may indicate the early stages of pressure sores. This vigilant monitoring is crucial for maintaining skin integrity and preventing potential complications
Reposition Frequently
Encourage movement, or reposition immobile individuals at least every two hours to effectively relieve pressure on vulnerable areas of the body. This practice is essential for preventing complications related to prolonged immobility, as regular shifting helps distribute weight more evenly and promotes overall comfort.
Keep Skin Clean and Moisture-Free
Maintain proper hygiene by utilizing gentle cleansers and effective moisture barriers to protect and care for the skin. It is essential to ensure that the skin remains clean and well-hydrated to prevent any irritations or damage.
Use Protective Devices
To effectively reduce pressure and shear forces on vulnerable areas of the body, it is essential to carefully apply cushions, specialized mattresses, or various other support surfaces. This thoughtful approach helps to enhance patient comfort and significantly decreases the risk of developing pressure sores.
Ensure Proper Nutrition
Adequate hydration, along with a well-balanced diet that is particularly rich in essential proteins and a variety of vitamins, is crucial for maintaining optimal skin health. Proper nutrition plays a significant role in promoting skin integrity and preventing issues such as dryness and irritation.
Preventive Tools and Strategies
-
Prophylactic Dressings
Special dressings for high-risk areas like heels and sacrum. These reduce pressure, friction, and moisture while protecting against infection.

-
Reminder Systems
Digital alerts integrated into care plans to prompt repositioning or skin checks, ensuring timely preventive actions.

Understanding Key Risk Factors
-
Staying in one position too long increases pressure on the skin, restricting blood flow and causing tissue damage. Regular repositioning is key to prevention.
-
Conditions like paralysis or nerve damage prevent individuals from feeling discomfort, making it harder to detect pressure sores early. Frequent skin checks are essential.
-
Sweat or incontinence softens and weakens the skin, making it more prone to breakdown. Keeping skin dry and using moisture barriers helps prevent sores.
-
A lack of essential nutrients slows healing and weakens skin, increasing the risk of sores. A diet rich in protein, vitamins, and hydration supports skin health.
Preventing Pressure Sores with Ease
-
Assess Current Position
Check which areas of the body are bearing pressure.
-
Determine New Position
Alternate between supine (lying on back), lateral (lying on side), and prone (lying on stomach, if possible).
-
Use Support Surfaces
Add pillows or foam supports to cushion bony areas and maintain alignment.
-
Document and Monitor
Record the repositioning time and note any signs of skin redness or irritation.
The Stages of Pressure Sores
Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar is removed, a Stage 3 orStage 4 pressure injury will be revealed. Stable eschar (i.e. dry, adherent, intact without erythema or (fluctuance) on the heel or ischemic limb should not be softened or removed.
Healthy skin - Lightly Pigmented
No Stage - No Pressure Injury:
The skin is intact, smooth, and free from any visible redness, discoloration, or wounds. It appears healthy with consistent tone and elasticity across all areas, showing no signs of moisture-associated damage, abrasions, or irritation. The skin feels supple, well-hydrated, and resilient to gentle pressure, indicating proper circulation and care. There are no indications of redness, blisters, or breaks in the skin, even over bony prominences like the pelvis or heels. Regular inspection and repositioning help maintain this healthy state.
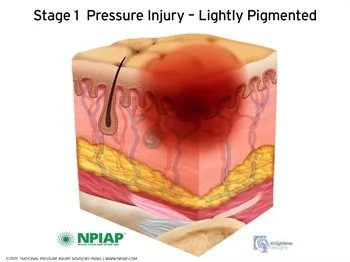
Stage 1 Pressure Injury:
Non-Blanchable Erythema of Intact Skin
Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes. Color changes do not include purple or maroon discoloration; these may indicate deep tissue pressure injury.
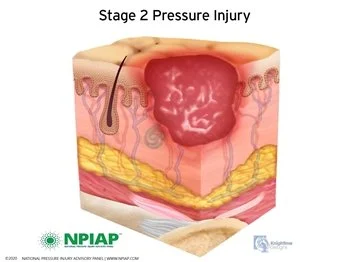
Stage 2 Pressure Injury:
Partial-thickness Skin Loss with Exposed Dermis
Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Adipose (fat) is not visible and deeper tissues are not visible. Granulation tissue, slough, and eschar are not present. These injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel. This stage should not be used to describe moisture-associated skin damage (MASD) including incontinence-associated dermatitis (IAD), intertriginous dermatitis (ITD), medical adhesive-related skin injury (MARSI), or traumatic wounds (skin tears, burns, abrasions).
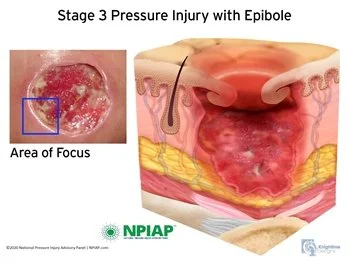
Stage 3 Pressure Injury:
Full-thickness Skin Loss
Full-thickness loss of skin, in which adipose (fat) is visible in the ulcer and granulation tissue and epibole (rolled wound edges) are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location; areas of significant adiposity can develop deep wounds. Undermining and tunneling may occur. Fascia, muscle, tendon, ligament, cartilage and/or bone are not exposed. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury.
Stage 4 Pressure Injury:
Full-thickness Skin and Tissue Loss
Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage or bone in the ulcer. Slough and/or eschar may be visible. Epibole (rolled edges), undermining and/or tunneling often occur. Depth varies by anatomical location. If slough or eschar obscures the extent of tissue loss this is an Unstageable Pressure Injury.
If you or a loved one are experiencing Stage 4 pressure injuries, you are highly encouraged to contact our team immediately. Join the movement for better care today!
Unstageable Pressure Injury:
Obscured Full-thickness Skin and Tissue Loss
A pressure injury is a localized skin and soft tissue damage, often over a bony area or from a medical device. It may appear as intact skin or an open ulcer and can be painful. Caused by prolonged pressure or shear, its severity is influenced by factors like microclimate, nutrition, circulation, and overall health.
Seek Support
To set up a free initial consultation to discuss your loved one’s condition, call us at 877-724-3476. You can also reach us using our online contact form.